Groundbreaking robotic surgery, Alzheimer’s blood test: 7 of the biggest medical breakthroughs in 2025
Written by ABC Audio ALL RIGHTS RESERVED on December 30, 2025

(NEW YORK) — From robotic surgery performed 7,000 miles away to the first blood test to help diagnose Alzheimer’s disease, 2025 has been a year full of medical breakthroughs.
Scientists discovered a brain implant to give some patients back their independence, prevented others from needing to take opioids and made a discovery that could help solve the organ shortage crisis.
Here are seven of the biggest innovations in the health and science space this year.
ALS patient is 1st to control iPad by thought with implantable brain sensor
A patient with amyotrophic lateral sclerosis (ALS) became the first person in the world to control an iPad entirely by thought, neurotech company Synchron announced earlier this year.
The patient, Mark Jackson, from western Pennsylvania, controls the tablet without using his hands or voice command but rather with an implantable brain-computer interface (BCI) that translates his thoughts into actions.
At the time, Jackson told ABC News he doesn’t have use of his arms so the BCI helps him watch TV shows, listen to audiobooks, browse social media and send text messages to his children.
BCIs are sensors implanted in the brain and translate brain signals into actions outside of the body. The BCI that Jackson is using was developed by the company Synchron, which involves a device implanted into one of the veins within the brain in a minimally invasive procedure.
“This is really an exciting field, because I think the opportunities are boundless,” Dr. Leah Croll, a neurologist at Maimonides Medical Center in New York City, told ABC News. “I think that we’re going to see, moving forward, not only using BCIs to control other electronic devices, but also using them to give patients back movement, to give patients back language, really bodily functions that they weren’t able to do after whatever neurologic insult happened to them.”
Croll said it’s important, going forward, to consider legal and ethical considerations such as privacy and data storage.
She also encouraged more research and clinical trials to generate data on how patients can be protected in both research and real-world settings.
“There’s so much we haven’t figured out legally and ethically when it comes to storing personal, private data from your brain, and how is that used, and how do we manage that responsibly,” she said. “There’s a lot of bio-ethical minds at work as to how we deal with this issue and how do we make it so that a patient isn’t sort of signing away the rights to their entire brain and inner world and manage something responsibly for them that’s helpful and not harmful.”
First pill for obstructive sleep apnea may be around the corner
The first oral pill for obstructive sleep apnea (OSA) could soon be available after a late-clinical showed positive results, according to pharmaceutical company Apnimed Inc.
The drug, AD109, showed “clinically meaningful and statistically significant reductions” in airway obstruction after 26 weeks, the company said in a press release in July.
OSA is a sleep disorder in which the airways become narrowed or blocked while sleeping, causing breathing to pause.
The investigational once-daily pill is a neuromuscular modulator that stabilizes upper airway muscles and prevents them collapsing, improving oxygenation.
OSA patients treated with the medication saw a nearly 50% reduction in the severity from baseline at week 26, compared to 6.8% of those in the placebo group.
The reduction was “significant” at the end of the study period, which concluded at 51 weeks. At the end of the trial, nearly 23% of participants saw “complete disease control.”
More recent trial data published in October found that a meaningful number of patients achieved complete disease control and experienced significant improvements in oxygenation measures.
First non-opioid medication in more than 20 years approved by FDA
Earlier this year, the FDA approved a new type of non-opioid pain medication to treat moderate to severe acute pain, the first of its kind on more than 20 years.
Suzetrigine, also known by the brand name, Journavx, is manufactured by biotech company Vertex Pharmaceuticals and doesn’t have addictive properties, unlike opioids often used for this type of pain.
“It’s significant in light of all the concerns about the opioid epidemic and addiction substance use disorder,” Dr. Jianguo Cheng, a professor of anesthesiology and medical director of the Cleveland Clinic Consortium for Pain at Cleveland Clinic, told ABC News.
In two clinical trials, tested on adults between ages 18 and 80, Journavx was found to reduce moderate to severe acute pain for adults from baseline by about 50% in 48 hours.
The average time to meaningful pain relief ranged from two to four hours, compared to eight hours in the placebo group, according to the trial.
Cheng, who was not involved in the clinical trials, said the studies demonstrated efficacy of the drug not compared to not only placebo, but also to weak opioids.
“Its efficacy is as good as a weak opioid. So why that is important?” Cheng said. “Because not all patients need opioids, and not all patients need a strong opioid. … If most of them do need a weak opioid, and if this can replace the weak opioid, that can be a big deal.”
Scientists discover immune reaction behind pig kidney rejection in transplant patients
Although gene-edited pig kidneys have been seen as a way to help ease the shortage of organs available for those on transplant waiting lists, many of the organs have been rejected not long after transplant surgery.
“Until 2021, we had never put one of these gene-edited pig organs into a human … so it was a bit of a mystery when we started doing the pig-to-human transplants, about what we were going to encounter,” Dr. Robert Montgomery, director of the NYU Langone Transplant Institute, told ABC News.
Last month, a team at NYU Langone Health published a study in which they discovered immune reactions that may explain why these organs get rejected.
The team collected two months of data from a patient who was brain dead and had a genetically engineered pig kidney transplanted into them. The family had donated the patient’s body to science.
The team learned that pig organs were being rejected due to an immune system reaction from specific antibodies — which recognize and attach themselves to foreign substances so they can be removed from the body — and from T cells, which are white blood cells that help the body fight off germs and other unfamiliar invaders.
‘So you have this very coordinated immune response that involves antibodies and white cells, and it seems to happen somewhere between two and four weeks after the transplant,” said Montgomery, lead author of the study. “Now the good news on that front is that we can detect when it’s coming before rejection happens, and we can begin to respond, and we have very good therapeutics that can block the rejection and prevent it from causing damage.”
After rejection, the team used an FDA-approved drug combination to successfully reverse it, with no signs of permanent damage or reduced kidney function.
In a second study, Montgomery and his team looked at the body’s immune response to the pig organ in greater detail. By measuring levels of biomarkers in the blood, they were able to spot an attack up to five days before it would be visible in bodily tissue.
Montgomery said the findings could lead to a future where gene-edited pig organs are a realistic alternative to human organs.
“The pig organ can really replace a human organ and do all the things that a human organ can do, and it’s really just a matter of overcoming the immunosuppression and preventing rejection,” he said. “I think it’s going to happen … and people will be receiving xenotransplants on a regular basis. It’s going to be normalized, and it’s going to be something that will benefit thousands, first, and then millions of people around the world.”
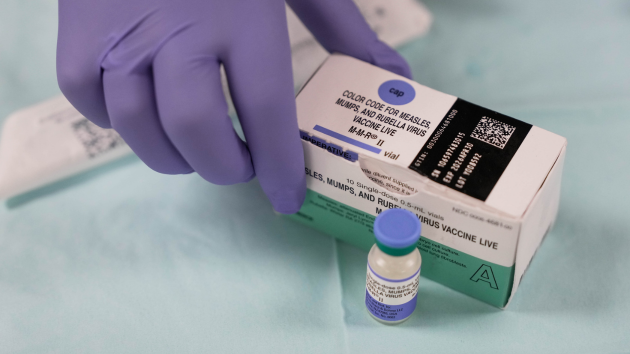
FDA clears 1st blood test to help diagnose Alzheimer’s disease
In May, the FDA cleared the first blood test to help diagnose Alzheimer’s disease.
The test, manufactured by Fujirebio Diagnostics, is for those aged 55 and older who are already exhibiting signs and symptoms of the disease, according to the federal health agency.
The new blood test works by measuring the ratio of two proteins — pTau217 and β-amyloid 1-42 — which are found in human plasma, a component of blood. That ratio is then linked to the presence or absence of amyloid plaques in the brain to determine whether a patient is showing signs of Alzheimer’s disease.
In a clinical study, more than 91% of nearly 500 cognitively impaired patients who tested positive on the blood test had their results confirmed by other diagnostic tools.
“Essentially, it does provide a first quantitative measure of an Alzheimer’s disease diagnosis,” Dr. Jeffrey Savas, an associate professor in the department of neurology at Northwestern University Feinberg School of Medicine, told ABC News. “This is very important to identify patients which could be good candidates for some of the emerging therapeutics.
Savas said the test is rapid, highly accurate and less expensive or invasive compared to previous diagnostic tests.
Because many Alzheimer’s patients need to wait months to see a specialist, the test can allow primary care providers to start the diagnostic process.
“Many neurological research centers have huge backlogs of patients, and there’s not enough physicians or nurses to really see the patients in a timely manner,” Savas said.
“Having this quick diagnostic test, which could be taken in other medical settings, should pave the way for quicker, more effective opportunities and chances for being treated in a timely manner.”
In October, the FDA cleared a second blood-based test called Elecsys pTau181, made by Roche.
Groundbreaking remote robotic surgery
A patient living in Angola with prostate cancer underwent surgery this year to cut the cancer out, but the doctor performing the surgery was 7,000 miles away in Orlando, Florida.
The patient was the first in a groundbreaking human clinical trial approved by the FDA to test transcontinental robotic telesurgery.
A team at OrlandoHealth operated on the patient via a multimillion-dollar robot with enhanced visuals and nimble controls.
Using a robot allows for the procedure to be less invasive, more precise and typically comes with a faster recovery time.
The team has said underserved areas in the U.S. and around the world could benefit from the technology by having a surgeon perform an operation even if they are not nearby.
1st-ever gene fix for rare deadly disease saves baby’s life
A baby with a rare and life-threatening metabolic disorder underwent a personalized treatment involving a first-of-its-kind type of gene-editing.
KJ Muldoon was diagnosed as a newborn with carbamoyl-phosphate synthetase 1 deficiency as a newborn. The disorder affects a bodily cycle that causes deadly levels of ammonia to build up in the blood, which can lead to severe and permanent brain damage.
If left untreated, it will typically result in the death of the patient, according to the National Organization for Rare Disorders.
The treatment for KJ involved the powerful gene-editing tool CRISPR, which allows scientists to precisely slice and repair faulty genes. Using CRISPR, the team was able to create a treatment tailored to the baby’s specific genetic mutation.
In June, KJ went home after spending the majority of his life at Children’s Hospital of Philadelphia. Earlier this month, he reached a big milestone: taking his first steps ahead of Christmas.
Copyright © 2025, ABC Audio. All rights reserved.
 KVSP
KVSP